CaseReport:
Rebuilding a Diagnostic Puzzle: Integrating History and Morphology
An 82-year-old male, who was asymptomatic, underwent follow-up for a simple kidney cyst by magnetic resonance imaging (MRI). A tumor on the lower lobule of the left lung was detected. A thoracic computed tomography showed the following findings:
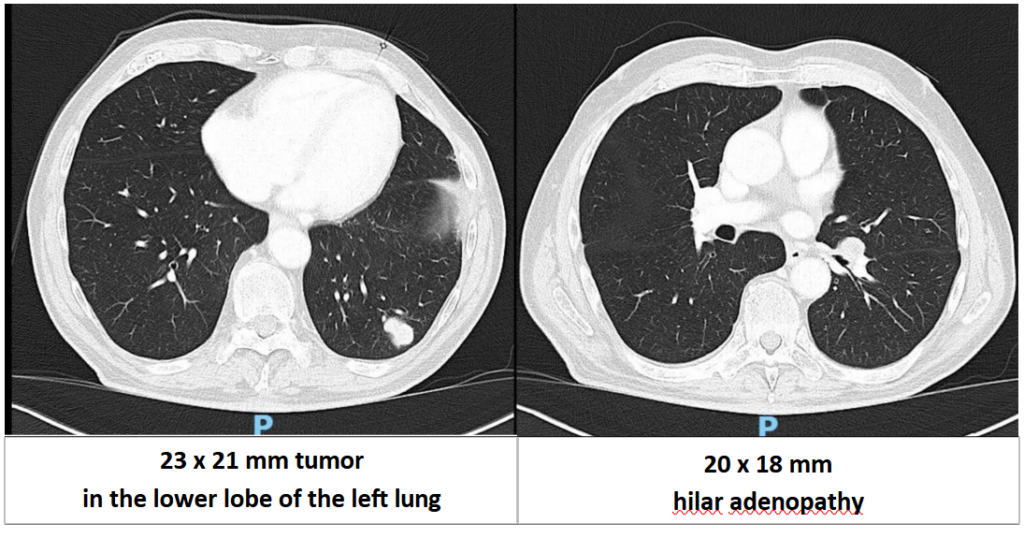
inthelowerlobeoftheleftlung
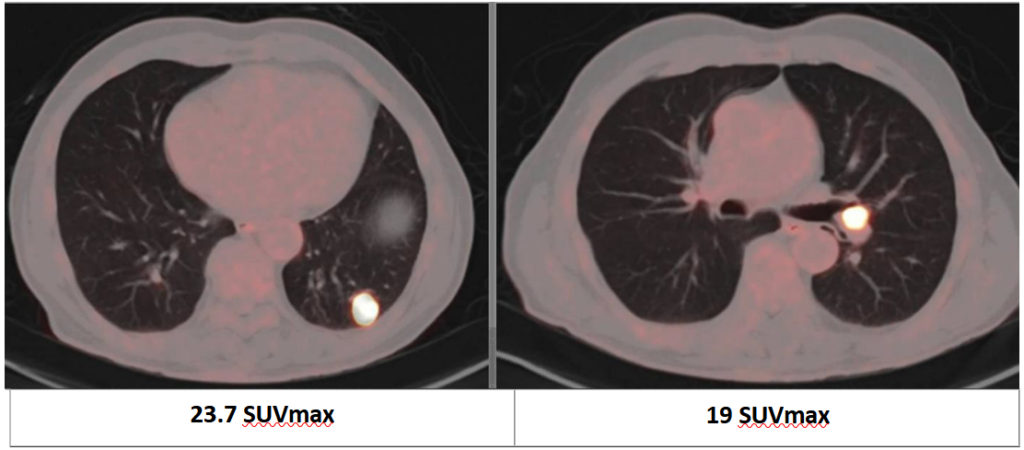
A full-body positron emission tomography (PET) scan was performed, revealing only the two previously mentioned lesions.
At this point, the patient denied any previous history of malignancy, so the clinician decided to perform an Endobronchial Ultrasound with Bronchoscope-Guided Fine-Needle Aspiration from the hilar adenopathy, under the suspicion that this would be a primary lung tumor. Aspirate smears and a cell block were obtained from the EBUS-B-FNA. Rapid On-Site Evaluation (ROSE) was performed.
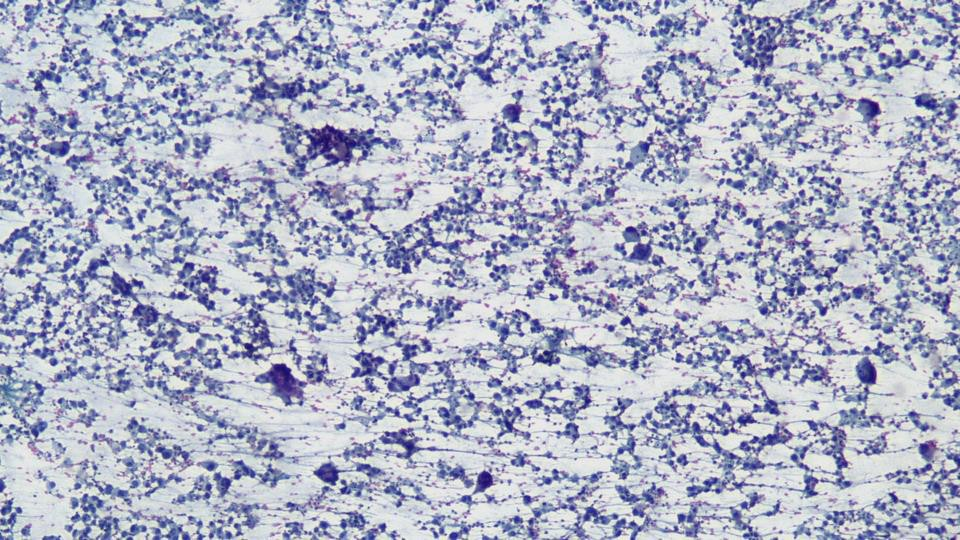
A poorly differentiated tumor, suspected of being a primary pulmonary neoplasm, was observed, so, initially, the following immunohistochemical studies were requested:
- TTF1
- Napsin A
- CK7
- CKAE1/AE3
- p40
All these markers where negative.
So, if you were thinking it was a poorly differentiated adenocarcinoma, and you see all these negative markers, you might be feeling a bit lost at this point, probably thinking of requesting a SMARCA4 determination.
But sometimes, it’s more important to review the clinical background before going further and requesting new immunohistochemical markers. So, we decided to ask the clinicians for further clinical details, including whether the patient was a smoker. They revealed that the patient had never been exposed to tobacco.
With this new information, we re-evaluated our diagnosis: what if this is not a primary tumor of the lung, but actually a metastasis?
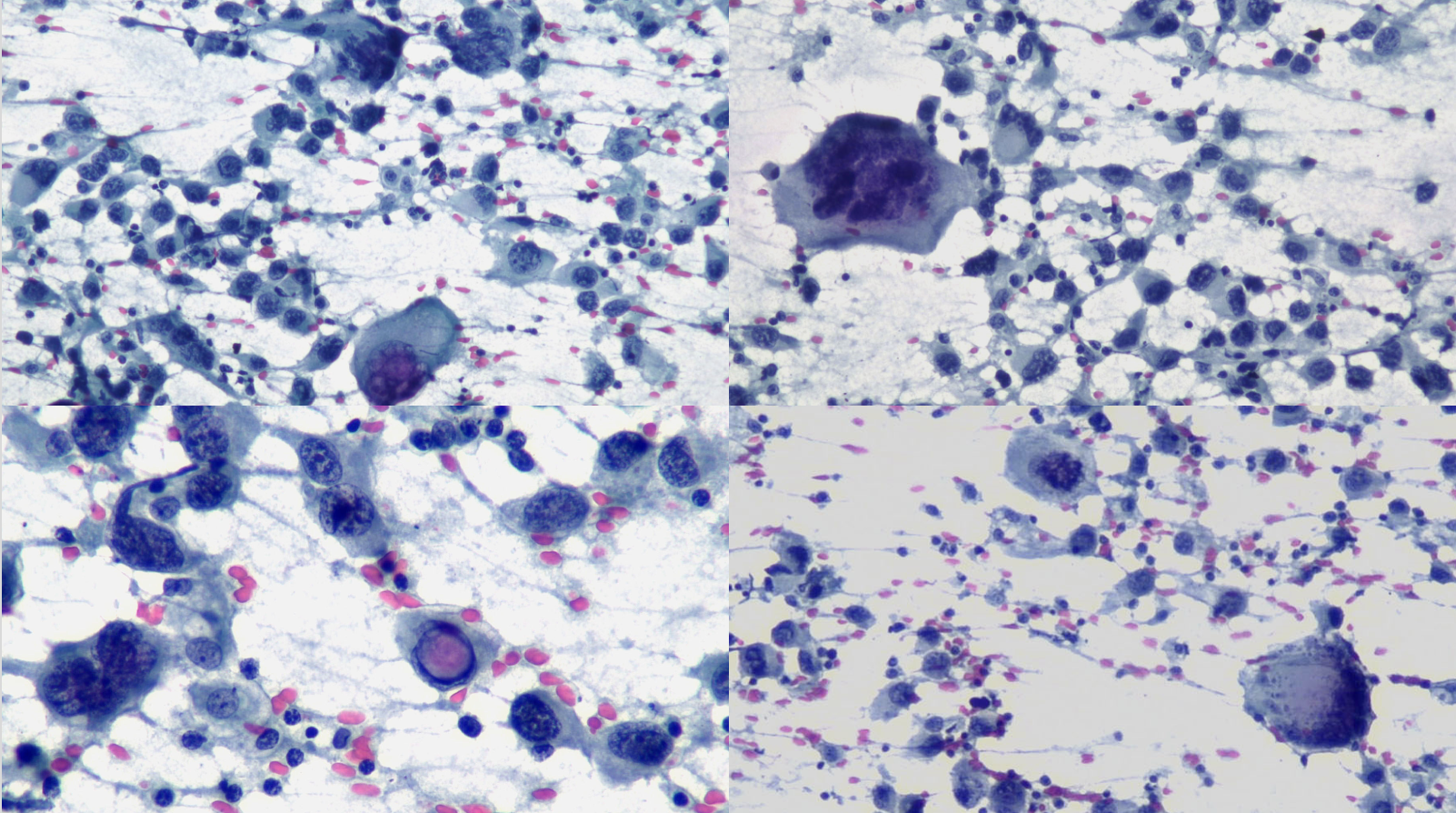
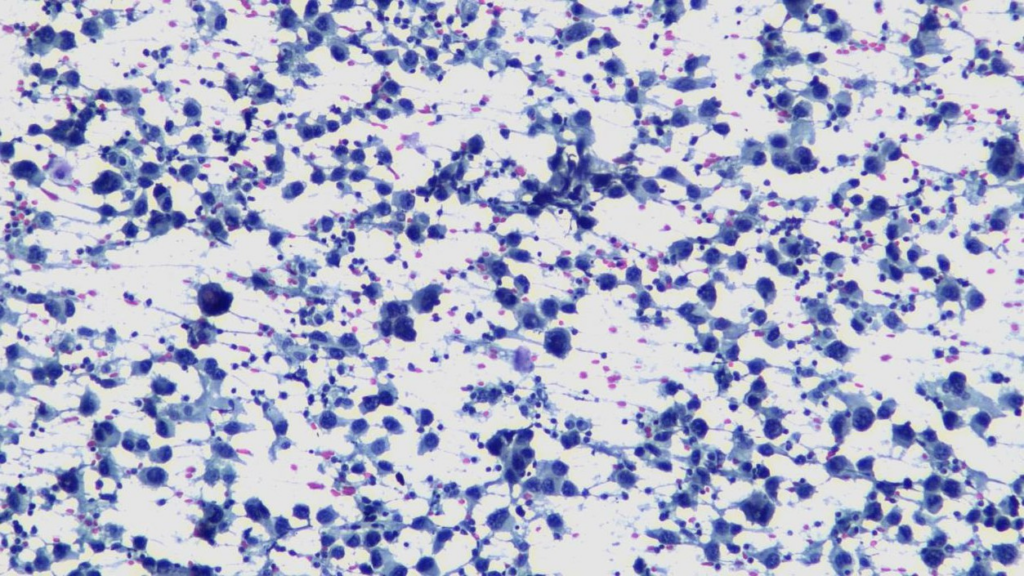
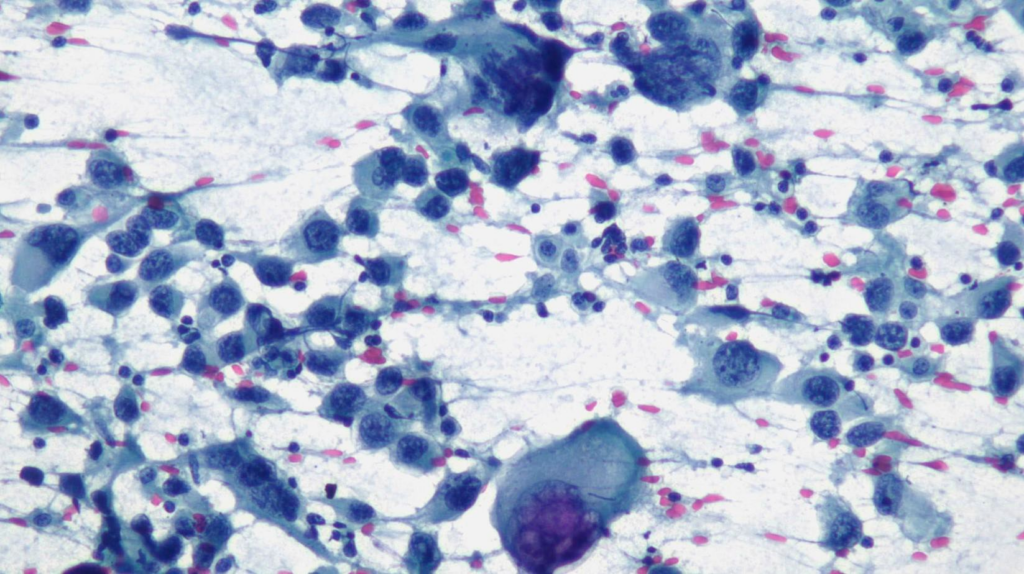
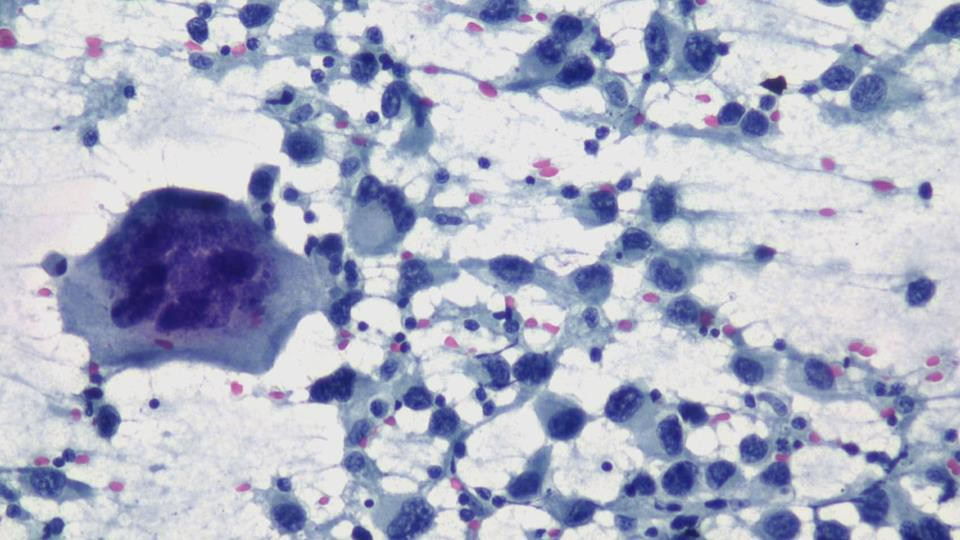
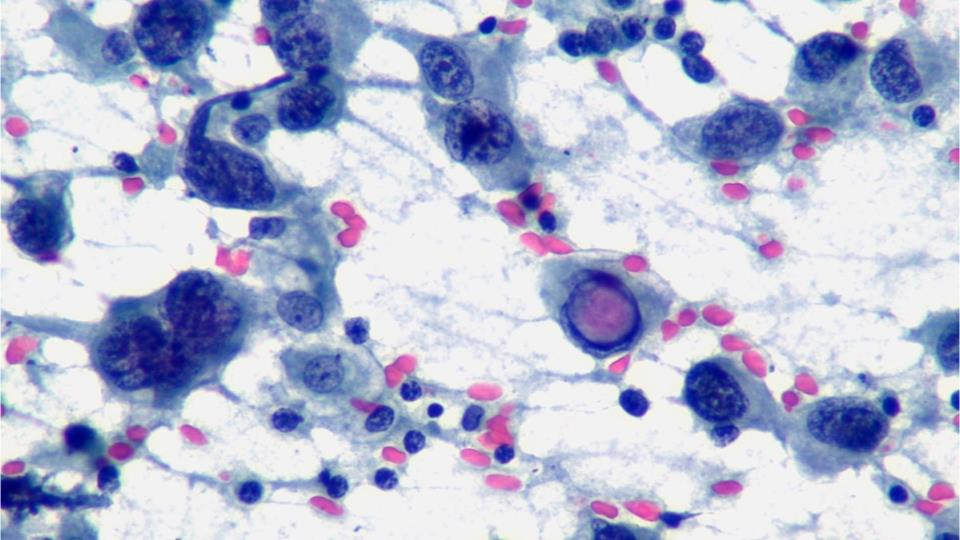
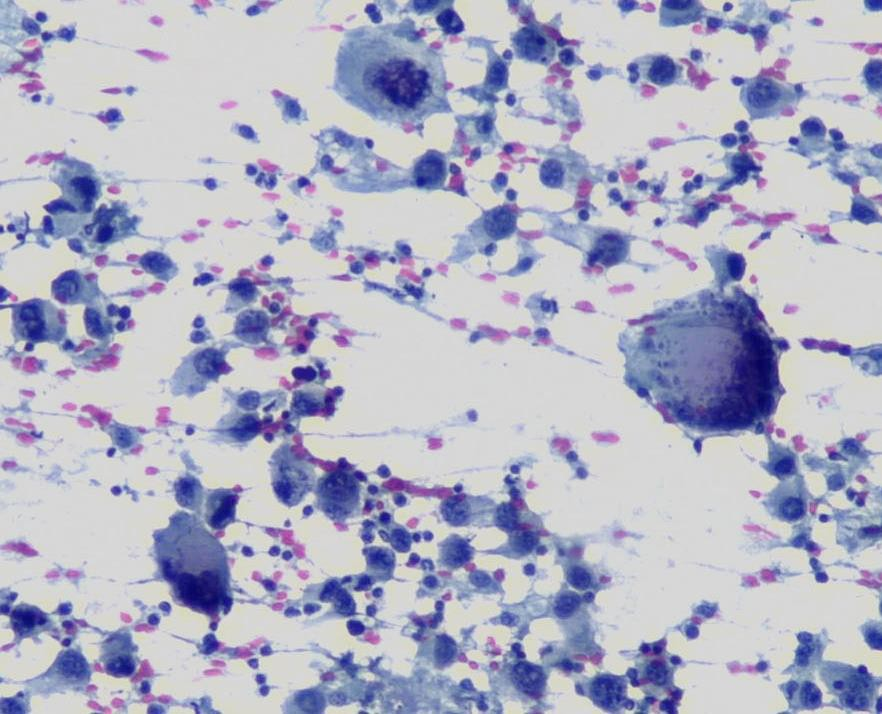
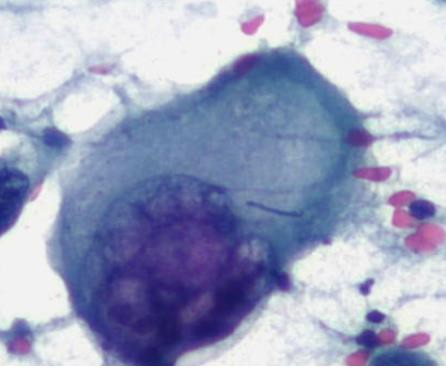
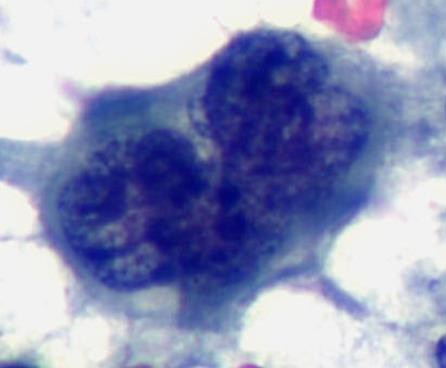
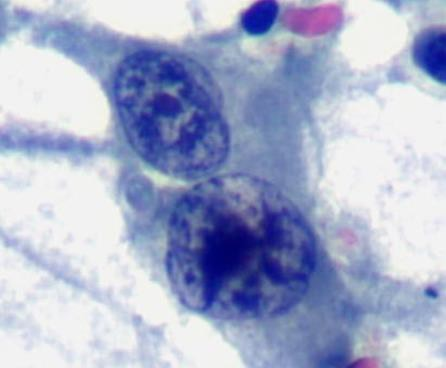
So, we started to look carefully at our cytological features:
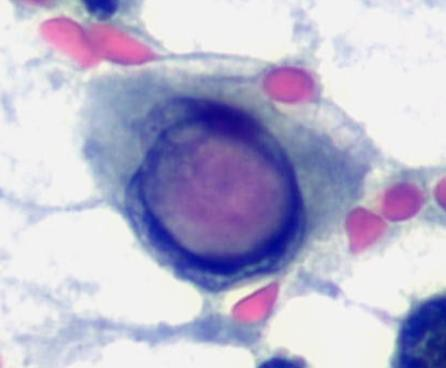
Given these cytological findings, we decided to request two other immunohistochemical markers:
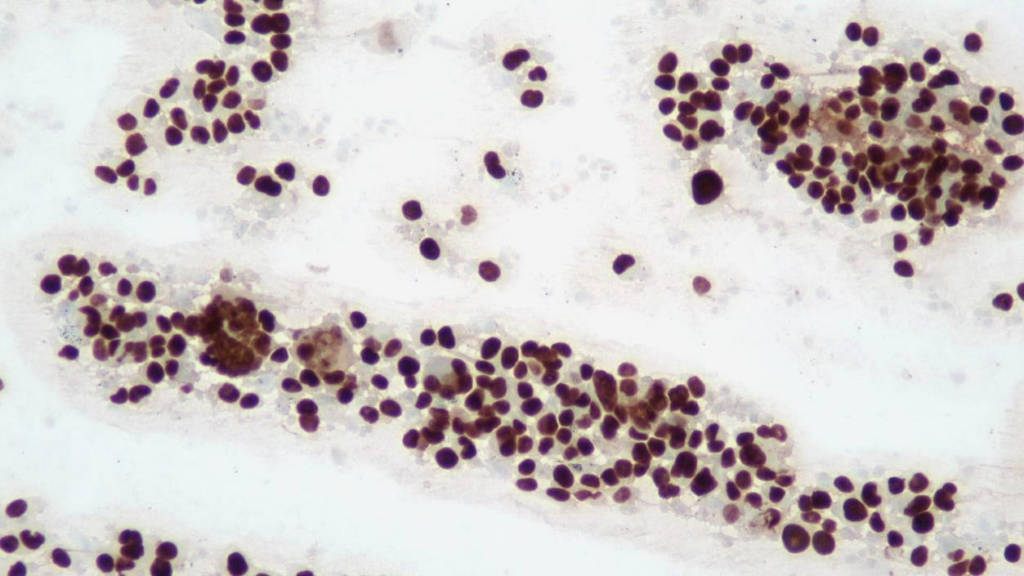
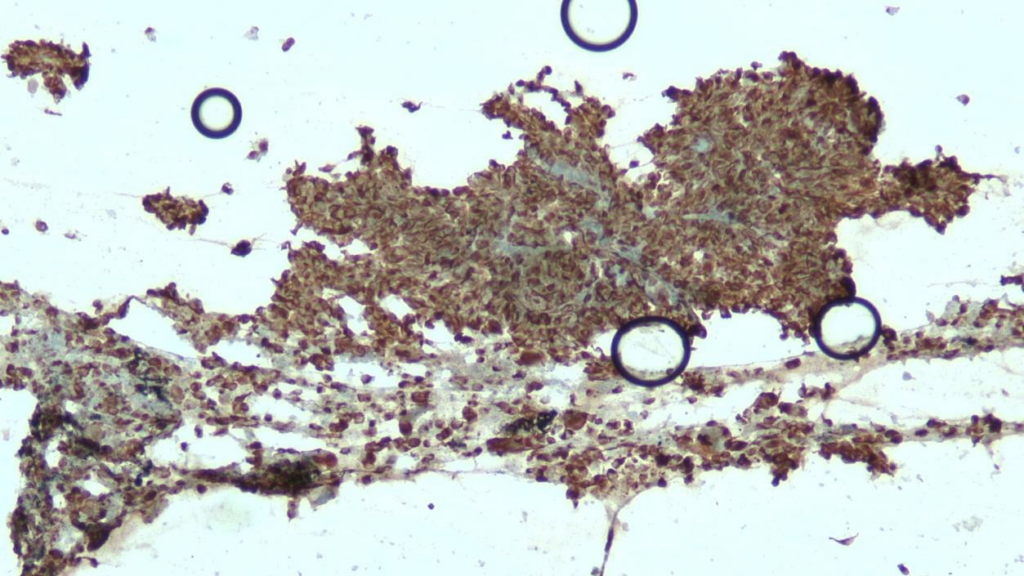
The final diagnosis was of metastasis of melanoma. The patient was referred to dermatology for a general examination, but only four nevi were identified, with no lesions consistent with melanoma. Although primary pulmonary melanoma is recognized in the 2021 WHO classification of pulmonary tumors, we believe this is most likely a metastasis from skin melanoma that has regressed.
Comment:
The clinical history of a patient is a fundamental aspect of pathological diagnosis. When working with pathological samples, understanding the patient’s medical background, symptoms, and risk factors provides crucial context for interpreting the findings. Without this information, it is easy to misinterpret or overlook certain diagnostic clues. Clinical history helps guide the differential diagnosis and ensures that all possible conditions, including rare or atypical ones, are considered. Therefore, a thorough review of the patient’s history is essential to reach an accurate diagnosis and provide the best possible care.
When working with our pathological samples, morphology should always be our first biomarker, before requesting any unnecessary immunohistochemical studies. Melanoma is the eternal mimic, the tumor that should consistently be considered in our differential diagnosis, as it can exhibit a wide range of nuclear patterns. However, it often presents with distinct features, such as prominent nucleoli, intranuclear cytoplasmic inclusions, binucleation, and may also contain cytoplasmic pigment.
Primary pulmonary melanoma (PPM) is an entity recognized in the 2021 World Health classification of lung tumors, which has been described in multiple publications dating from 1916, and is classified in a group termed “tumors of ectopic origin”, which encompass tumors that are more common presented in other sites, but sometime can arise as primary pulmonary tumors. The actual existence of this entity is doubted, and the most accepted theory to this day attempting explain these tumors is that they are a metastases from a primary cutaneous melanoma with regression, a well-described phenomenon.
Author of the case
Allan Argueta, MD Special thanks to M.D. Lozano M.D., Ph.D. for her support in the developing of this case.
REFERENCES
Nicholson AG, Tsao MS, Beth Beasley M, Borczuk AC, Brambilla E, Cooper WA, et al. The 2021 WHO Classification of Lung Tumors: Impact of Advances Since 2015. J Thorac Oncol [Internet]. 2022 [cited 2023 Jan 20];17(3):362–87. Available from:
Yang C, Sanchez-Vega F, Chang JC, Chatila WK, Shoushtari AN, Ladanyi M, et al. Lung-only melanoma: UV mutational signature supports origin from occult cutaneous primaries and
argues against the concept of primary pulmonary melanoma HHS Public Access. Mod Pathol [Internet]. 2020 [cited 2023 Jan 20];33(11):2244–55. Available from:
Sekine I, Kodama T, Yokose T, Nishiwaki Y, Suzuki K, Goto K, et al. Rare pulmonary tumors – a review of 32 cases. Oncology [Internet]. 1998 [cited 2023 Jan 21];55(5):431–4. Available